
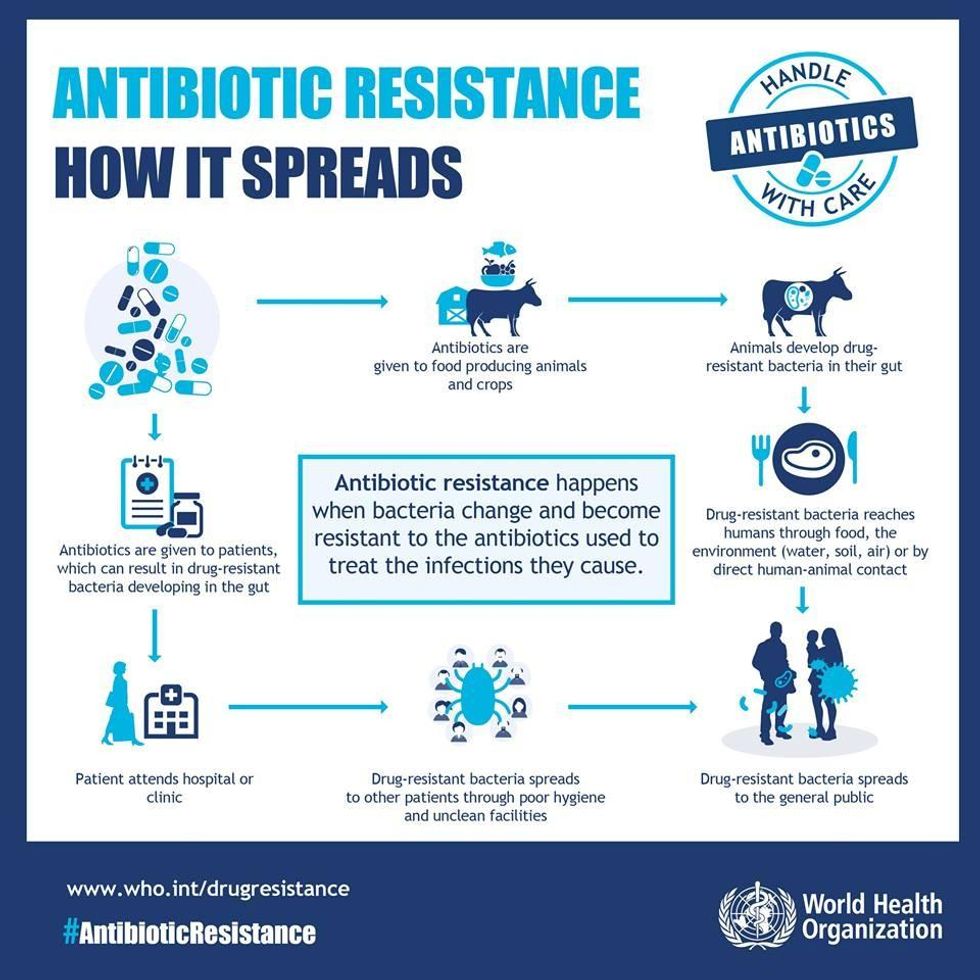
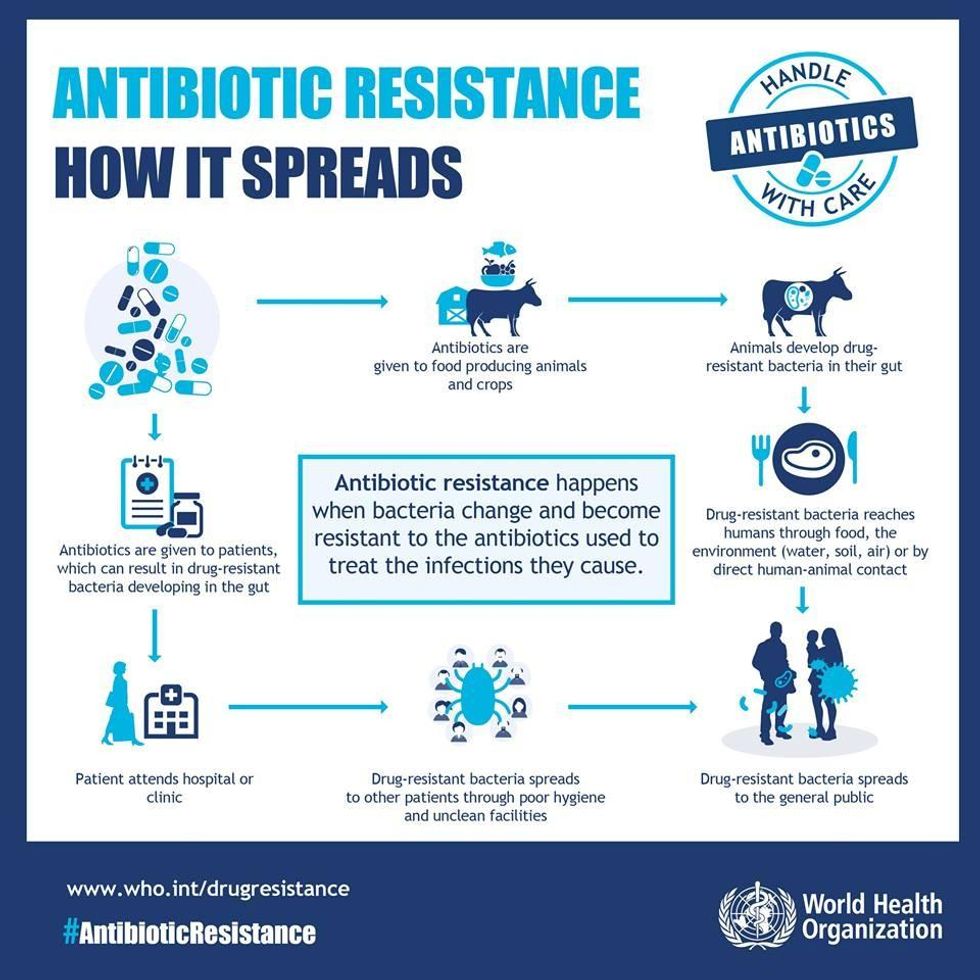
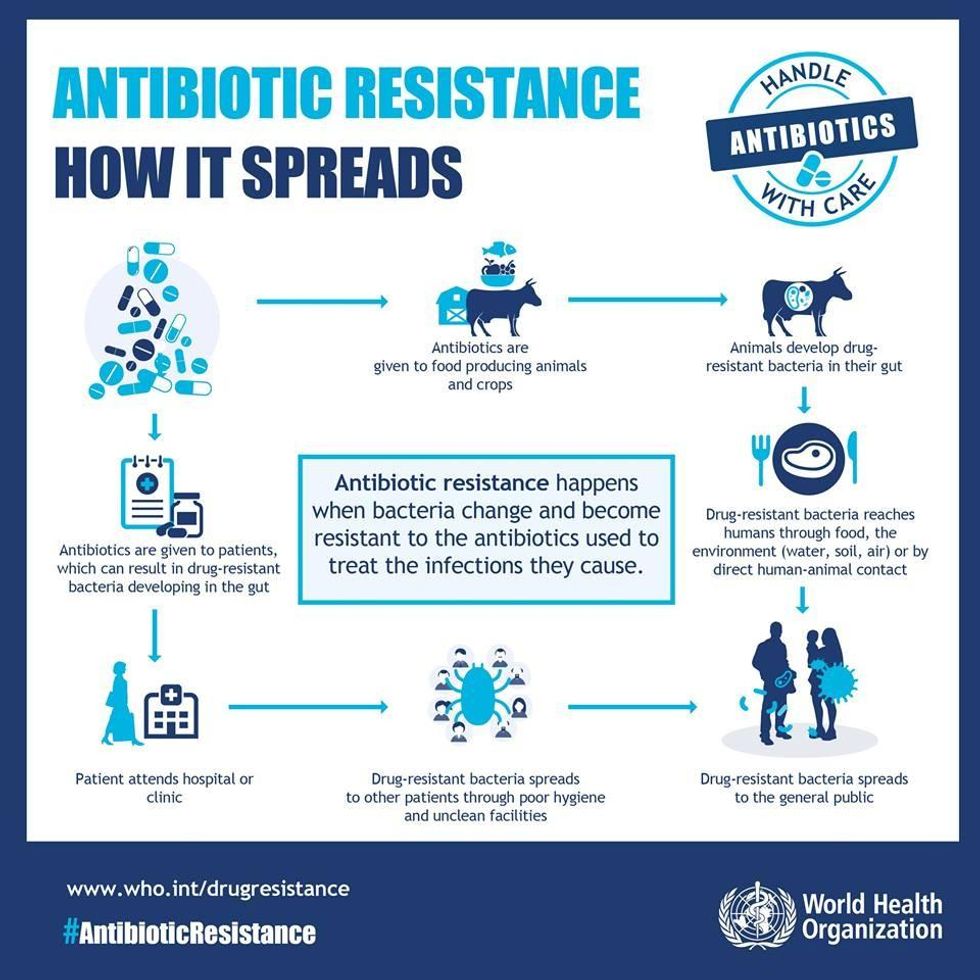
The World Health Organization issued formal guidelines instructing farmers significantly antibiotic use in healthy livestock, responding to growing fears about the threat of antibiotic resistance. (Photo: Center for Food Policy/Twitter)
To Fight Global Threat of Antibiotic Resistance, WHO Issues First-Ever Guidelines to Curb Use
Experts warn without urgent action on a global scale, "by 2050, almost all current antibiotics will be ineffective in preventing and treating human disease"
To address the major and growing global threat that stems from rampant overuse and misuse of antibiotics in agriculture, the World Health Organization (WHO) this week issued its first-ever formal guidelines instructing farmers to stop using so many antimicrobials in healthy livestock.
"As important as these guidelines are, they are just that--guidelines. To help curb resistance, individual companies and/or countries actually have to take action on them."
--David Wallinga, NRDC
"If no action is taken today, by 2050, almost all current antibiotics will be ineffective in preventing and treating human disease, and the costs of losing these drugs will exceed U.S. $100 trillion in terms of national productivity," the U.N. agency predicts in a related policy brief (pdf).
David Wallinga, a senior health officer at the Natural Resources Defense Council (NRDC), said the guidelines "may be a game-changer in this fight," because they call for "fairly significant changes to how many of the world's biggest food-animal producers now operate, including the U.S."--but "as important as these guidelines are, they are just that--guidelines. To help curb resistance, individual companies and/or countries actually have to take action on them."
The U.S.-based advocacy group Center for Food Safety (CFS) welcomed the guidelines, while also noting how they "illustrate the degree to which our regulators and large food animal producers are falling short."
Cameron Harsh, CFS's senior manager for organic and animal policy, called on the U.S. Food and Drug Administration (FDA) to reconsider its support for using antibiotics on livestock for disease prevention, urging the FDA to "better align domestic policies with the WHO and to take stronger measures to restrict and reduce use of antibiotics in food animals raised in the U.S."
The WHO guidelines reflect growing concerns about the amount of antibiotics used in agriculture, and what that means for both humans and animals in the long term.
As Kazuaki Miyagishima, director of the WHO's Department of Food Safety and Zoonosesn, explains: "the volume of antibiotics used in animals is continuing to increase worldwide, driven by a growing demand for foods of animal origin," and "scientific evidence demonstrates that overuse of antibiotics in animals can contribute to the emergence of antibiotic resistance."
WHO Director-General Tedros Adhanom Ghebreyesus warns that "a lack of effective antibiotics is as serious a security threat as a sudden and deadly disease outbreak."
"Driven by the need to mitigate the adverse human health consequences of use of medically important antimicrobials in food-producing animals," the guidelines (pdf) include four recommendations:
- An overall reduction in use of all classes of medically important antimicrobials in food-producing animals;
- Complete restriction of use of these antimicrobials in food-producing animals for growth promotions;
- Complete restriction of use for prevention of infectious diseases that have not yet been clinically diagnosed; and
- Antimicrobials classified by the WHO as "highest priority critically important" for human medicine should not ever be used to treat food-producing animals, while antimicrobials classified as "critically important" should not be used to control the dissemination of an infection within a group of food-producing animals.
Since 2005, WHO has published a list of antimicrobials categorized as "important," "highly important," or "critically important" to human medicine, with the goal of preserving the effectiveness of available antibiotics. The latest revision (pdf) was published in April 2017.
The guidelines also feature two best practice statements. In the first, the WHO declares that "any new class of antimicrobials or new antimicrobial combination developed for use in humans will be considered critically important for human medicine unless otherwise categorized by WHO."
The second statement advises that "medically important antimicrobials that are not currently used in food production should not be used in future production including food-producing animals or plants," acknowledging that although the guidelines focus on livestock rather than plants, using antibiotics on plants also contributes to antimicrobial resistance that can be transferred to humans.
The guidelines were released just ahead of U.S. Antibiotic Awareness Week--an annual effort by the Centers for Disease Control and Prevention (CDC) to raise awareness about antibiotic resistance--which begins November 13. The CDC found that as of 2013, more than 2 million Americans are infected with antibiotic-resistant bacteria each year, and about 23,000 of those people die because of the infection.
An Urgent Message From Our Co-Founder
Dear Common Dreams reader, The U.S. is on a fast track to authoritarianism like nothing I've ever seen. Meanwhile, corporate news outlets are utterly capitulating to Trump, twisting their coverage to avoid drawing his ire while lining up to stuff cash in his pockets. That's why I believe that Common Dreams is doing the best and most consequential reporting that we've ever done. Our small but mighty team is a progressive reporting powerhouse, covering the news every day that the corporate media never will. Our mission has always been simple: To inform. To inspire. And to ignite change for the common good. Now here's the key piece that I want all our readers to understand: None of this would be possible without your financial support. That's not just some fundraising cliche. It's the absolute and literal truth. We don't accept corporate advertising and never will. We don't have a paywall because we don't think people should be blocked from critical news based on their ability to pay. Everything we do is funded by the donations of readers like you. Will you donate now to help power the nonprofit, independent reporting of Common Dreams? Thank you for being a vital member of our community. Together, we can keep independent journalism alive when it’s needed most. - Craig Brown, Co-founder |
To address the major and growing global threat that stems from rampant overuse and misuse of antibiotics in agriculture, the World Health Organization (WHO) this week issued its first-ever formal guidelines instructing farmers to stop using so many antimicrobials in healthy livestock.
"As important as these guidelines are, they are just that--guidelines. To help curb resistance, individual companies and/or countries actually have to take action on them."
--David Wallinga, NRDC
"If no action is taken today, by 2050, almost all current antibiotics will be ineffective in preventing and treating human disease, and the costs of losing these drugs will exceed U.S. $100 trillion in terms of national productivity," the U.N. agency predicts in a related policy brief (pdf).
David Wallinga, a senior health officer at the Natural Resources Defense Council (NRDC), said the guidelines "may be a game-changer in this fight," because they call for "fairly significant changes to how many of the world's biggest food-animal producers now operate, including the U.S."--but "as important as these guidelines are, they are just that--guidelines. To help curb resistance, individual companies and/or countries actually have to take action on them."
The U.S.-based advocacy group Center for Food Safety (CFS) welcomed the guidelines, while also noting how they "illustrate the degree to which our regulators and large food animal producers are falling short."
Cameron Harsh, CFS's senior manager for organic and animal policy, called on the U.S. Food and Drug Administration (FDA) to reconsider its support for using antibiotics on livestock for disease prevention, urging the FDA to "better align domestic policies with the WHO and to take stronger measures to restrict and reduce use of antibiotics in food animals raised in the U.S."
The WHO guidelines reflect growing concerns about the amount of antibiotics used in agriculture, and what that means for both humans and animals in the long term.
As Kazuaki Miyagishima, director of the WHO's Department of Food Safety and Zoonosesn, explains: "the volume of antibiotics used in animals is continuing to increase worldwide, driven by a growing demand for foods of animal origin," and "scientific evidence demonstrates that overuse of antibiotics in animals can contribute to the emergence of antibiotic resistance."
WHO Director-General Tedros Adhanom Ghebreyesus warns that "a lack of effective antibiotics is as serious a security threat as a sudden and deadly disease outbreak."
"Driven by the need to mitigate the adverse human health consequences of use of medically important antimicrobials in food-producing animals," the guidelines (pdf) include four recommendations:
- An overall reduction in use of all classes of medically important antimicrobials in food-producing animals;
- Complete restriction of use of these antimicrobials in food-producing animals for growth promotions;
- Complete restriction of use for prevention of infectious diseases that have not yet been clinically diagnosed; and
- Antimicrobials classified by the WHO as "highest priority critically important" for human medicine should not ever be used to treat food-producing animals, while antimicrobials classified as "critically important" should not be used to control the dissemination of an infection within a group of food-producing animals.
Since 2005, WHO has published a list of antimicrobials categorized as "important," "highly important," or "critically important" to human medicine, with the goal of preserving the effectiveness of available antibiotics. The latest revision (pdf) was published in April 2017.
The guidelines also feature two best practice statements. In the first, the WHO declares that "any new class of antimicrobials or new antimicrobial combination developed for use in humans will be considered critically important for human medicine unless otherwise categorized by WHO."
The second statement advises that "medically important antimicrobials that are not currently used in food production should not be used in future production including food-producing animals or plants," acknowledging that although the guidelines focus on livestock rather than plants, using antibiotics on plants also contributes to antimicrobial resistance that can be transferred to humans.
The guidelines were released just ahead of U.S. Antibiotic Awareness Week--an annual effort by the Centers for Disease Control and Prevention (CDC) to raise awareness about antibiotic resistance--which begins November 13. The CDC found that as of 2013, more than 2 million Americans are infected with antibiotic-resistant bacteria each year, and about 23,000 of those people die because of the infection.
To address the major and growing global threat that stems from rampant overuse and misuse of antibiotics in agriculture, the World Health Organization (WHO) this week issued its first-ever formal guidelines instructing farmers to stop using so many antimicrobials in healthy livestock.
"As important as these guidelines are, they are just that--guidelines. To help curb resistance, individual companies and/or countries actually have to take action on them."
--David Wallinga, NRDC
"If no action is taken today, by 2050, almost all current antibiotics will be ineffective in preventing and treating human disease, and the costs of losing these drugs will exceed U.S. $100 trillion in terms of national productivity," the U.N. agency predicts in a related policy brief (pdf).
David Wallinga, a senior health officer at the Natural Resources Defense Council (NRDC), said the guidelines "may be a game-changer in this fight," because they call for "fairly significant changes to how many of the world's biggest food-animal producers now operate, including the U.S."--but "as important as these guidelines are, they are just that--guidelines. To help curb resistance, individual companies and/or countries actually have to take action on them."
The U.S.-based advocacy group Center for Food Safety (CFS) welcomed the guidelines, while also noting how they "illustrate the degree to which our regulators and large food animal producers are falling short."
Cameron Harsh, CFS's senior manager for organic and animal policy, called on the U.S. Food and Drug Administration (FDA) to reconsider its support for using antibiotics on livestock for disease prevention, urging the FDA to "better align domestic policies with the WHO and to take stronger measures to restrict and reduce use of antibiotics in food animals raised in the U.S."
The WHO guidelines reflect growing concerns about the amount of antibiotics used in agriculture, and what that means for both humans and animals in the long term.
As Kazuaki Miyagishima, director of the WHO's Department of Food Safety and Zoonosesn, explains: "the volume of antibiotics used in animals is continuing to increase worldwide, driven by a growing demand for foods of animal origin," and "scientific evidence demonstrates that overuse of antibiotics in animals can contribute to the emergence of antibiotic resistance."
WHO Director-General Tedros Adhanom Ghebreyesus warns that "a lack of effective antibiotics is as serious a security threat as a sudden and deadly disease outbreak."
"Driven by the need to mitigate the adverse human health consequences of use of medically important antimicrobials in food-producing animals," the guidelines (pdf) include four recommendations:
- An overall reduction in use of all classes of medically important antimicrobials in food-producing animals;
- Complete restriction of use of these antimicrobials in food-producing animals for growth promotions;
- Complete restriction of use for prevention of infectious diseases that have not yet been clinically diagnosed; and
- Antimicrobials classified by the WHO as "highest priority critically important" for human medicine should not ever be used to treat food-producing animals, while antimicrobials classified as "critically important" should not be used to control the dissemination of an infection within a group of food-producing animals.
Since 2005, WHO has published a list of antimicrobials categorized as "important," "highly important," or "critically important" to human medicine, with the goal of preserving the effectiveness of available antibiotics. The latest revision (pdf) was published in April 2017.
The guidelines also feature two best practice statements. In the first, the WHO declares that "any new class of antimicrobials or new antimicrobial combination developed for use in humans will be considered critically important for human medicine unless otherwise categorized by WHO."
The second statement advises that "medically important antimicrobials that are not currently used in food production should not be used in future production including food-producing animals or plants," acknowledging that although the guidelines focus on livestock rather than plants, using antibiotics on plants also contributes to antimicrobial resistance that can be transferred to humans.
The guidelines were released just ahead of U.S. Antibiotic Awareness Week--an annual effort by the Centers for Disease Control and Prevention (CDC) to raise awareness about antibiotic resistance--which begins November 13. The CDC found that as of 2013, more than 2 million Americans are infected with antibiotic-resistant bacteria each year, and about 23,000 of those people die because of the infection.

