In June 22, 2017, Alec Raeshawn Smith, a recently promoted restaurant manager with Type 1 diabetes, left his local pharmacy empty-handed. He'd gone in to pick up a month's worth of insulin supplies, which he assumed would set him back around $1000--the amount he and his mother Nicole Smith-Holt had budgeted the month before when he turned 26 and, under Obamacare rules, had to drop off her insurance coverage.
For Alec, that price was already steep: Even with his promotion, he was making $35,000 a year with no benefits. He and Smith-Holt had combed through Minnesota's Obamacare marketplace for months in search of a decent plan, but the affordable ones all had sky-high deductibles. That meant that he'd be paying full price for his insulin for months before his junk insurance kicked in, on top of hundreds of dollars in monthly premiums--sucking up some 80 percent of his take-home pay once he paid the rent. So he made a rational decision: He'd go uninsured, save the cost of the premium, and just pay for his meds out of pocket, while racking up work experience that could serve as a springboard to a better position with health insurance.
As it turned out, it wouldn't have made a difference if Alec had been insured or not: The price of his insulin had apparently gone up again to $1300, which was more than he had in his bank account. Perhaps he felt embarrassed, too proud to borrow money so soon after finally moving out of his parents' place. Perhaps he didn't want anyone to worry about him, and figured he could keep his blood sugar down until payday.
So he left. He never told his mother and he never told his girlfriend. Five days later, he was dead.
The autopsy later determined the cause of death to be ketoacidosis, a complication of diabetes typically brought about by not taking insulin. Recounting hearing the news of her son's death, Smith-Holt didn't quite put everything together at first, wondering if Alec had inadvertently taken too much insulin, inducing hypoglycemic shock. "Rationing insulin never even crossed my mind," she told me. "It wasn't until later, when the medical examiner said to me that Alec had absolutely no insulin left in the apartment whatsoever--every single pen he picked up was completely empty. And he was amazed by how many pens looked like they had been tampered with ... like he was trying to extract whatever little bit was left in them."
In the two years since her son's death, Smith-Holt has fought alongside diabetes patients and their allies to make insulin the public face of the drug-pricing crisis. The story of how an otherwise healthy young adult could die of a $300 shortfall in an apartment full of mutilated insulin cartridges in the richest country on earth is a hundred years in the making. It's a story of what happens when a country delegates both the provision and financing of lifesaving drugs to an oligopolistic private industry, and then prioritizes that sector's business interests above patients. If the grassroots organizers of the #insulin4all campaign get their way, it will become the story of how the diabetes community can force a political reckoning with the ever-rising prescription drug costs that dominate their lives.
TODAY, SOME 30 MILLION Americans are living with diabetes, a chronic disease caused by the pancreas being unable to properly metabolize carbohydrates, leading to high blood sugar levels. Likely cases--judging by a telltale constellation of symptoms including weight loss, frequent urination, and insatiable thirst--are speckled throughout medical texts dating back to antiquity, but were virtually untreatable until the 20th century. For most of its history, a diabetes diagnosis carried with it a death sentence within mere months, a duration that could be prolonged only slightly with near-starvation diets that kept blood sugars low by practically eliminating food (the tactic Holt imagined her son must have tried when he couldn't afford his meds).
Fortunately, a modern diabetic's outlook is far sunnier. A patient can expect to live for decades if their disease is properly managed. For seven million Americans, treatment entails several daily doses of insulin, a synthetic version of the hormone excreted by a healthy pancreas. For Type 1 diabetes patients, uninterrupted access to insulin is especially critical. Their health outcomes depend heavily not only on taking proper doses, but on minimizing variance between blood sugar levels--an imperative that demands a vigilant routine of measurement and monitoring, often facilitated by supplies and multiple variations of insulins. As Type 1 patient Laura Marston described to me the ongoing balancing act: "Imagine you have to live your entire life just as you do today, but you have to play a game of Tetris 24/7 on your cellphone."
It's not a game that T1 patients can opt out of: Just a few days without insulin can be deadly, or trigger severe complications like gangrene or renal failure. But its crippling cost makes a mechanized routine increasingly difficult to pull off. Most T1 diabetics use two or three vials of fast-acting insulin a month, plus a secondary basal insulin, on top of any necessary supplies. But the wholesale prices of the most common insulins tripled from 2007 to 2017. The three pharmaceutical companies that manufacture insulin--Lilly, Novo Nordisk, and Sanofi--rake in billions in profits annually from insulin sales alone, with the U.S. market accounting for 15 percent of global insulin users but almost 50 percent of its worldwide revenues. Insulin ranks among each company's top-selling drugs; one BMJ study showed that prices could be slashed considerably and the drugs would still be profitable.
Media coverage tends to frame skyrocketing insulin prices as a betrayal of the miracle drug's origins, the definitive account of which was offered by historian Michael Bliss in his 1982 classic The Discovery of Insulin. In 1922, months of exhaustive experimentation surgically removing dogs' pancreases to induce diabetes and re-injecting them with an extract made from their former organs finally vindicated the efforts of an orthopedist named Frederick Banting and his small University of Toronto lab team. Not only did their extract keep diabetic dogs alive far longer than the unfortunate control group, but the injections also revitalized human patients so close to death they'd consented to participate in small-scale trials as a last resort.
Realizing the significance of their drug, three members of the Toronto team sold their patent rights to the university for $1 apiece in an effort to protect its integrity from greedy commercial enterprises. That included a pharmaceutical company in Indianapolis called Eli Lilly and Company, which had expressed interest in manufacturing insulin for humans as soon as they caught wind of the Toronto team's research. Having refused to cooperate with Lilly, Banting and his colleagues believed they were protecting future access.
Determined to prevent insulin from becoming a business racket, the Toronto team kept Lilly at bay through months' worth of repeated attempts to collaborate. The university had been doing its best to manufacture insulin on its own, but struggled to meet the demands of even the small group of patients participating in early trials. What limited supply it did produce was subject to shortages and contamination, which Lilly reps were all too happy to emphasize in making their case that a professional, scaled-up manufacturing operation was in the best interests of diabetes patients. Eventually, Banting and his team reluctantly agreed: Lilly was granted exclusive rights to manufacture and distribute insulin in the United States for one year, with European rights going to a Danish firm called Nordisk (later merged to become Novo Nordisk, as it is known today). Thereafter, both firms were entitled to patent any future innovations on their products, and competitors were hypothetically free to enter the market.
FOR NEARLY A HALF-CENTURY, the price stayed relatively affordable for U.S. patients. Arguably, it was precisely this lack of price-gouging that allowed Lilly to maintain de facto dominance over the U.S. insulin market even after their period of exclusivity had ended: Rival firms had no real incentive to compete with an already entrenched, scaled-up manufacturer whose prices were already relatively low. Moreover, there was reason to believe the Department of Justice was prepared to intervene on behalf of exploited diabetes patients, after leveling small antitrust violation fines in 1941 to three players in Lilly's insulin supply chain.
The delicate circumstantial balance that kept insulin prices low for years began to wobble in the 1970s, when a broader neoliberal turn in politics set the stage for the pharmaceutical industry to become the single most profitable sector in the American economy. The Institutional Patent Agreement program introduced by the National Institutes of Health in 1968, as well as the Bayh-Dole Act of 1980, created pathways for private entities to patent and commercialize public research. This emboldened the profit motive within science. Meanwhile, mid-century breakthroughs in DNA sequencing were on the cusp of paying off in the form of groundbreaking new drugs, at the very moment that both speculative investment and maximizing shareholder value became Wall Street dogma. All of this sparked staggering investment in pharmaceutical companies.
For insulin manufacturers, recombinant DNA technology promised to shake up a market that had been relatively placid since the days of Frederick Banting. Insulins had become more purified and precise, but remained fundamentally similar to the pork and bovine versions produced since the 1920s. That changed in 1982, when Eli Lilly debuted Humulin--the first so-called "human insulin," made out of bacteria instead of animal pancreas. Just as it was going off-patent, the company introduced a new fast-acting insulin called Humalog in 1996. Patent evergreening is also common; Sanofi, whose insulin product is called Lantus, has filed 74 different patent applications on just that one drug, meaning it could go without competition for 37 years. As of 2014, the top three insulin manufacturers held 19 active patents on insulins alone.
While research suggests that the new, more expensive insulins offered minimal benefits for many users (particularly those with Type 2 diabetes), Lilly's aggressive marketing campaigns--combined with partnerships with newer, more convenient delivery devices--convinced a majority of health-care providers to prescribe the costliest available medicines. With back-to-back exclusivity patents precluding generic competition for decades, insulin prices began to climb. In 1996, diabetes patient Laura Marston recalled her mother paying $25 for her first-ever vial of Humalog; the same dose runs $275 today.
If it's difficult to pinpoint the exact moment the price-gouging began, it's easy to see how it ends: with patients like Alec Smith dying of arbitrary price hikes that break already stretched budgets. Since her son's death, Nicole Smith-Holt told me, she's met five or six other parents who lost diabetic children at age 26, after they'd become uninsured. Other people she met were fortunate enough to get the drugs they needed, but still described how dramatically ever-rising insulin costs impacted their lives. "You know, I've heard of people having to sell all their possessions or relocate where rent is more affordable," Smith-Holt recounted. "I've heard of people staying at jobs they don't want just to have insurance coverage. I've heard of people dropping out of college, I've heard of people cashing in their retirement just to keep their spouse or child alive ... I've heard of people my age having to move in with their children because they can't afford to live independently with the rising cost of insulin. I've heard of people reaching out through the black market and buying questionable products in dark alleys."
Such desperation isn't just anecdotal: One study recently published in JAMA Internal Medicine found that one in four diabetes patients reports rationing their insulin due to costs. Lead author Dr. Kasia Lipska told me her study was inspired by increasing complaints from clinic patients, who would beg her not to prescribe higher doses for financial reasons. "It's a terrible, terrible situation," she told me by phone. "The conversations are heart-wrenching because the truth is as a clinician I have few choices. It makes me so angry because I wish I could do more."
And however striking her study's results may have been, Lipska stressed that they didn't capture the extent of her subjects' suffering: "That one-in-four number only reflects people who actually used less insulin because of costs, but other people make trade-offs," she explained. "They may be spending less on food or other necessary items, even on other medications."
THE ASTRONOMICAL COSTS STRAINING Lipska's patients and all the others I've talked to stem from a very obvious problem. In the United States, drug companies have near-unilateral power to name their own price, and insulin manufacturers don't face significant competition that might compel them to lower prices. In other industrialized countries, regulatory bodies are more stringent when it comes to which drugs they approve for sale, and aggressively negotiate prices with manufacturers. In the United States, drugmakers need only to prove their drug effective against a placebo rather than existing products, and the government is far less involved in pricing. In the case of Medicare Part D, government negotiating of drug prices is explicitly illegal.
Instead, U.S. drug-pricing negotiations are the responsibility of individual insurance plans, of which there are thousands. Each of them has relatively little leverage against price hikes, which drug manufacturers have every reason to push as high as possible to pay off shareholders, whose investments were predicated on the promise of some of the highest returns in the stock market. If you're a pharma exec whose goal is to maximize short-term profits, then jacking up prices on a drug like insulin--whose millions of patients are practically captive--is a sensible strategy.
Because private insurers are fundamentally ill equipped to negotiate drug prices, another for-profit industry began to rise in the late 1970s promising to do better. So-called pharmacy benefit managers, or PBMs, act on behalf of multiple insurers to negotiate with drug companies as a group, which theoretically gives them more leverage to buy in bulk. But there's mounting evidence that this isn't how PBMs work--because they often get paid in rebates from drug manufacturers, they're often incentivized to keep prices high, the opposite of what they exist to do. Lilly has claimed that, despite rising prices, the price it has been paid for Humalog fell over the past five years, because of all the rebates captured by the PBMs.
Finally, as insurance companies feel the squeeze of rising drug and health-care costs and strive to maximize profits of their own, they've shifted more and more health-care costs onto policyholders themselves. Average deductibles have quadrupled in the past decade, nearly half of all people with employer-based insurance have high-deductible plans, and co-pays have risen or been replaced with coinsurance, a frequently higher percentage of the overall price. Taken altogether, the deterioration of insurance quality and rising list prices mean that individual patients are bearing more and more of the brunt of high drug costs. In other words, $275 isn't just the jumping-off point for an opaque back-and-forth negotiation between Lilly and insurers; it's the amount that untold numbers of diabetics pay out of pocket for a few days worth of medication to stay alive.
At this point, defenders of the pharmaceutical industry would likely point out that high drug prices are a necessary evil to recoup R&Dcosts and facilitate innovation. Extremely high industry profit margins, the fact that pharmaceutical marketing budgets exceed those for R&D, and the relative lack of genuine drug innovation in recent years all cast doubt on this argument. But Lipska is particularly skeptical of it when it comes to insulin. "We're not even talking about rising prices for better products here," she said. "I want to make it clear that we're talking about rising prices for the same product ... there's nothing that's changed about Humalog. It's the same insulin that's just gone up in price and now costs ten times more."
And even when pharma companies do invest in R&D (Lilly sank at least $40 million into developing what would become Humulin, according to a 1980 article in Science), they depend on the vast annals of knowledge unlocked by publicly funded scientific discovery. Government is often the only entity with the will to pursue the long, careful research that would make quarterly profit-seeking executives bristle. "There's a highly symbiotic relationship between publicly funded science and industry-developed innovation," explained Dr. Jing Luo, the lead author on several papers on insulin pricing. "Recombinant human insulin could not have been introduced by Eli Lilly without the discovery of recombinant DNA technology. Where does that come from? None of it is possible without sequencing DNA, or the technologies used to do science around DNA ... you can't do innovation without standing on the giants of publicly funded science."
In a statement, a spokesperson for Novo Nordisk said, "We know that as the healthcare system has changed a growing number of Americans with diabetes struggle to pay for their healthcare, including medicines made by us. As a company focused on improving the lives of people with diabetes, this is not acceptable ... we are focused on doing all we can so these patients can afford their medicine." Lilly and Sanofi did not respond to a request for comment.
There is one proven method for lowering prices: fomenting robust generic competition after the drug goes off-patent. Lilly's patent on fast-acting insulin expired in 2014, but because insulin is a "biologic" drug made from human genetic material as opposed to a simple molecule, manufacturing a biosimilar version is relatively complicated and far from guaranteed to drive prices down. And drug companies fight to keep their exclusivity: When Merck tried to create a biosimilar to Sanofi's Lantus, Sanofi sued and Merck eventually dropped the effort. (Another biosimilar was ultimately approved in 2016, but not until after a similar patent lawsuit.)
But if only one generic enters the market, it typically doesn't make a big price difference--the biosimilar version of Lantus is priced at only 15 percent below the name brand. Studies show that the market price sees a dramatic reduction only after the entry of several generic competitors into the market--begging the question of whether waiting out two decades of exclusivity, followed by the mobilization of numerous different companies to eventually compete prices down, is really the best route to humane drug pricing.
Plenty of politicized diabetes patients like Laura Marston in Washington, D.C., can't afford to wait that long, and have taken up the fight themselves. "We all live this way," she said. "I'm scared all the time. I'm scared if I don't keep fighting they'll just go back to raising the prices. We're almost being forced to fight for our lives because the government won't do it for us, and the toll that takes on someone who already has a chronic illness is time consuming ... because even though I have a stable job, even though I'm insured, god forbid my industry could go in the tank tomorrow ... this is America! Anything can happen."
THOUSANDS OF DIABETES PATIENTS and their allies have joined the #insulin4all campaign, begun by nonprofit T1International in 2014 to force a national dialogue on insulin prices. Advocates have organized rallies at Lilly's Indianapolis headquarters, shaming the company into releasing its own licensed genericHumalog at half price. This is still over $100 per vial more than it sold for in 1996. Lilly's generic is also only available out of pocket; insurers will only be able to get Humalog at full price, with much of that burden passed on in patient deductibles--and more broadly, into our premiums.
Advocates have also forced congressional hearings on insulin, a federal investigation from House Oversight Committee Chair Elijah Cummings, at least two active lawsuits for price fixing, and even state legislation like the recently passed co-pay cap on insulin in Colorado. The law is a nice start, but applies only to state-regulated employer insurance plans and will thus shut out many diabetics who need it, like those in non-qualifying plans or the uninsured.
Other players in the insulin supply chain are scrambling as well. Sanofi has set a fixed price of $99 per month for monthly supplies, but also only for patients paying cash. Express Scripts, one of the largest PBMs, recently created a program to lower out-of-pocket insulin costs; again, this covers only a small section of the patient population, and health plans have to affirmatively pick up the option. Walmart sells an old version of human insulin for $25, but as Lipska explained, it doesn't work for all patients and is incompatible with many new delivery devices. Patient outrage is driving these moves, but they mostly amount to half measures.
As one blogger noted, the recent Colorado legislation--along with most of the measures listed here--doesn't pass the Alec Smith test. Removing all financial barriers to insulin to ensure that all patients have an uninterrupted supply of it would require governmental intervention, not just relying on multinational companies to devise better deals. It might even demand making moves that end our reliance on those firms to make the drugs we need most. Elizabeth Warren has written legislation providing for the public manufacturing of generic drugs, and explicitly stated in the bill that generic insulin would have to be produced within a year of passage. Even President Obama's former head of Medicare and Medicaid, Andy Slavitt, has recommended the total nationalization of the insulin market.
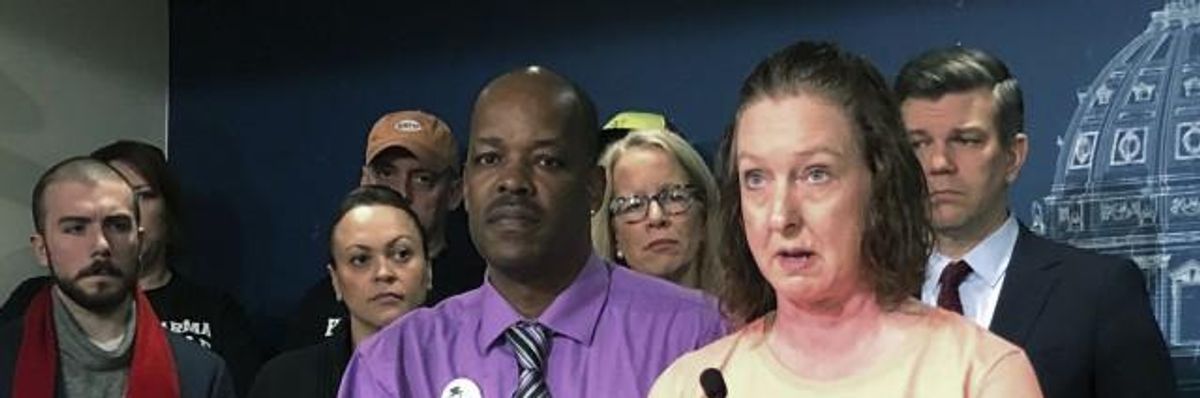
For her part, Nicole Smith-Holt no longer has a relative who needs insulin, but has stayed to fight for others. In early May, she joined eight members of the Minnesota chapter of #insulin4all on a so-called "Caravan to Canada"--a five-hour road trip across the border to demonstrate the pressures on diabetes patients in the United States. Once they arrived, the same vials of insulin that retail for nearly $300 here were being sold for $30 apiece.
Smith-Holt didn't need any insulin, but bought some as a memento. "If I had known that by driving five hours north that I could have saved my son's life for a couple hundred dollars, then he would still be here," she told me after the trip. "Because I would have crawled, I would have swam, I would have biked, I would have done whatever I had to do to get there."