
A health worker shows a bottle of Moderna Covid-19 vaccine for medical staff at Adam Malik hospital on August 4, 2021 in Medan, Indonesia. (Photo: Ivan Damanik/NurPhoto via Getty Images)
To donate by check, phone, or other method, see our More Ways to Give page.

A health worker shows a bottle of Moderna Covid-19 vaccine for medical staff at Adam Malik hospital on August 4, 2021 in Medan, Indonesia. (Photo: Ivan Damanik/NurPhoto via Getty Images)
A quiet monthslong legal fight between the U.S. National Institutes of Health and drugmaker Moderna over COVID-19 vaccine patents recently burst into public view. The outcome of the battle has important implications, not only for efforts to contain the pandemic but more broadly for drugs and vaccines that could be critical for future public health crises.
I teach drug regulation and patent law at Saint Louis University's Center for Health Law Studies.
Moderna recently offered to share ownership of its main patent with the government to resolve the dispute. Whether or not this is enough to satisfy the government's claims, I believe the dispute points to serious problems in the ways U.S. companies bring drugs and vaccines to market.
Vaccines have played a crucial role in the response to the pandemic.
In December 2020, Moderna became the second pharmaceutical company after Pfizer to obtain authorization from the Food and Drug Administration to market a COVID-19 vaccine in the United States. People have since grown so used to talking about the "Moderna vaccine" that a crucial element in the history of how it was developed risks being overshadowed: Moderna was not the sole developer of the vaccine.
Unlike many of the other pharmaceutical companies involved in the COVID-19 vaccine race, Moderna is a newcomer to drug and vaccine commercialization. Founded in Massachusetts in 2010, the company had never brought a product to market until the FDA authorized its COVID-19 vaccine last year.
Throughout the 2010s, Moderna focused on the development of mRNA technology, attracting over US$2 billion in funding from pharmaceutical companies and other investors. It went public in 2018.
Even before the pandemic, research on both coronaviruses and vaccine candidates against emerging pathogens was a priority for agencies operating in the public health space. In 2015, the National Institute of Allergy and Infectious Diseases, an institute within the NIH, signed a cooperative R&D agreement with Moderna on basic research, including the development of new vaccines. The agreement resulted in an undisclosed amount of funding and assistance with research.
In addition, after the COVID-19 outbreak began Moderna also received almost $1 billion in funding from the Biomedical Advanced Research and Development Authority, which operates within the Department of Health and Human Services. This funding was specifically targeted to the development of a COVID-19 vaccine candidate.
Researchers have calculated that, collectively, the U.S. government has provided $2.5 billion toward the development and commercialization of Moderna's COVID-19 vaccine.
In addition to providing financial support, the federal government was instrumental in the development of Moderna's vaccine for other reasons. Namely, federal scientists worked alongside Moderna scientists on different components of the vaccine.
These contributions included working on dosing mechanisms, and the NIH said federal scientists created the stabilized spike proteins that are a key component of the vaccine made by Moderna.
The importance of the role played by federal scientists in their work with Moderna would soon become apparent. A 2019 agreement with a third party explicitly acknowledged this, alluding to mRNA vaccine candidates "developed and jointly owned by NIAID and Moderna." And by late 2020, the U.S. government was calling it the "NIH-Moderna COVID-19 vaccine."
While the U.S. government has spent money on COVID-19 vaccines made by other companies, its close involvement in the R&D stages of Moderna's sets it apart.
As development of the vaccine progressed, Moderna applied for several patents, each one covering different components of the vaccine. U.S. law allows inventors to apply for patents on products or methods that are new, not obvious and useful. While some early modern vaccines--like the polio vaccine developed by Jonas Salk's team--were not covered by patents, from the late 20th century onward it became very common for one or multiple patents to cover a newly developed vaccine.
In applying for some patents related to its vaccine, Moderna named National Institute of Allergy and Infectious Diseases scientists as co-inventors alongside Moderna scientists. This was the case, for example, in a patent application dated May 2020 for a relatively minor component of the vaccine.
However, in July 2021, Moderna made it clear that it would not name government scientists as co-inventors in a patent application covering a much more significant component of the vaccine: the mRNA sequence used to produce the vaccine, known as mRNA-1273.
Moderna's position was that Moderna scientists alone had selected the sequence. The company informed the Patent and Trademark Office of its position in a 2020 statement.
In November 2021, government officials publicly challenged the company's decision after months of failed negotiations with the company. Moderna then took to social media to defend its position, tweeting:
"Just because someone is an inventor on one patent application relating to our COVID-19 vaccine does not mean they are an inventor on every patent application relating to the vaccine."
\u201cOur official statement on intellectual property. Thread.\u201d— Moderna (@Moderna) 1636663102
By contrast, the National Institutes of Health argued that three NIAID scientists--Kizzmekia Corbett, Barney Graham and John Mascola--had meaningfully contributed to the invention, though they've declined to publicly specify how. If true, patent law says they should be named co-inventors.
But this dispute is not merely about scientific principles or technical aspects of the law. While patents are also regarded as proxies for measuring scientific reputation, their most immediate and powerful effect is to give patent holders a significant amount of control over the covered technology--in this case, the main component of the vaccine made by Moderna.
From a practical perspective, excluding federal scientists from the application means that Moderna alone gets to decide how to use the vaccine, whether to license it and to whom. If, by contrast, the government co-owns the vaccine, federal patent law allows each of the joint owners to engage in a variety of actions--from making and selling the vaccine to licensing it--without the consent of the other owners.
This is especially relevant in cases of product scarcity or potential pricing issues in connection with the commercialization of the vaccine. For instance, the U.S. would have the ability to allow more manufacturers to produce vaccines using the mRNA-1273 technology. In addition, it could direct vaccine doses wherever it likes, including to lower-income countries that have received few vaccines so far.
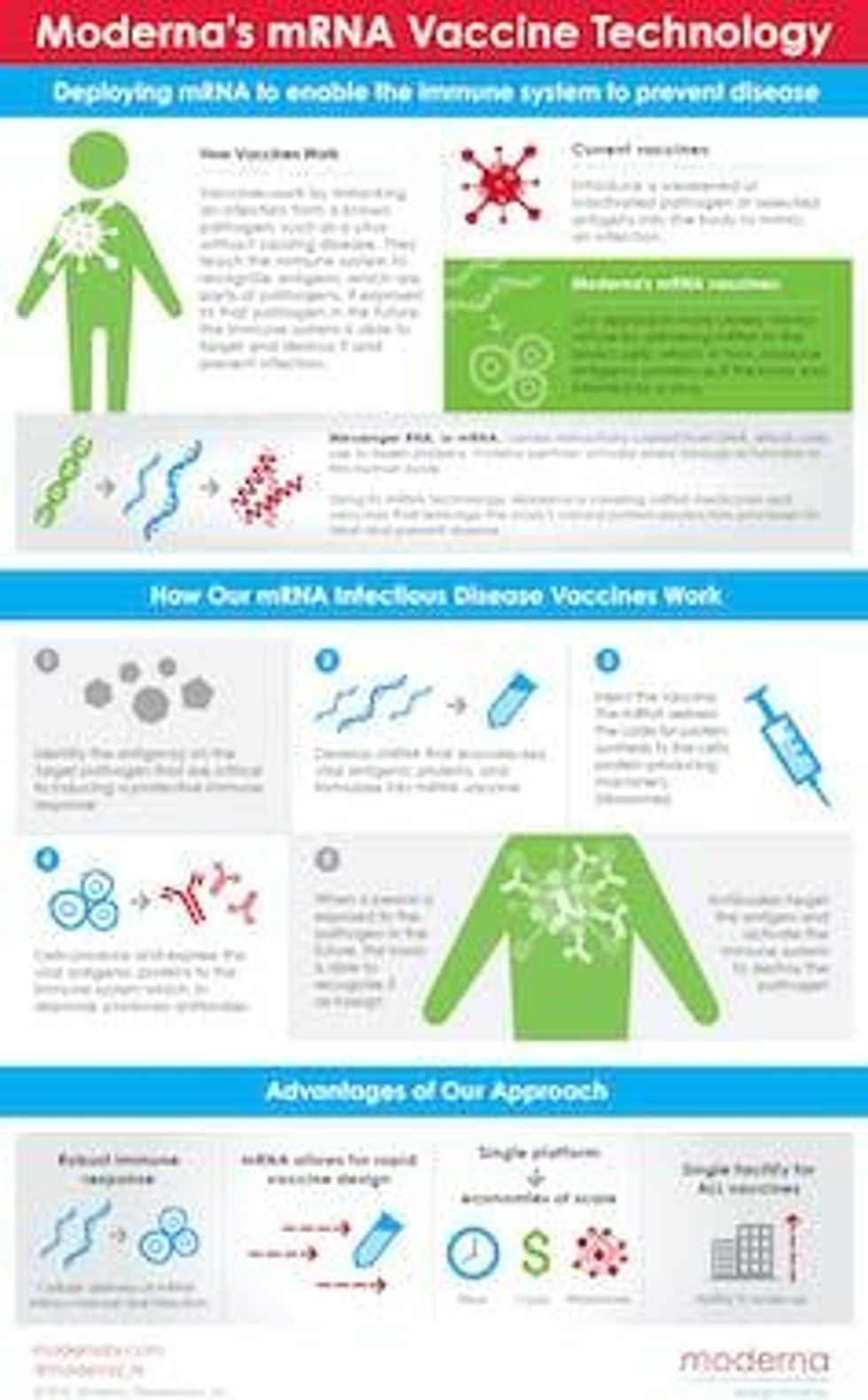 Moderna explains its mRNA technology. (Business Wire)
Moderna explains its mRNA technology. (Business Wire)The ongoing battle between the government and an emerging star in the pharmaceutical industry is yet another episode in a complicated relationship between actors with complementary yet distinct roles in the production of drugs and vaccines.
On the one hand, the federal government has long played a critical role in both performing and funding basic research. On the other, it does not have the resources and capacity to bring most types of new drugs and vaccines to market on its own.
The pharmaceutical industry thus plays an important and necessary role in drug innovation, which I believe should be rewarded--although not boundlessly.
If the NIH is correct about co-ownership of the vaccine, then Moderna is unduly using a legal tool to achieve a position of market control--a reward it does not deserve. This position of sole control becomes even more problematic in light of the significant amounts of public money that funded the development of this vaccine. This offset some of Moderna's financial risk, even as the company projects to make $15 billion to $18 billion in revenue from vaccine sales in 2021 alone, with much more expected in 2022.
However, even if the NIH prevails in the patent dispute, it is important to understand the limitations of such a "win." The U.S. would be in a position to license the vaccine, for example, and could do so by requiring that licensees agree to equitable distribution of vaccine doses.
But co-ownership would not enable the government to fix any of the other problems that currently affect the manufacturing and distribution of COVID-19 vaccines, such as scaling up production or building infrastructure to deliver vaccine doses.
In my view, the dispute is a reminder of the many problems embedded in how vaccines are made and delivered in the U.S. And it shows that when taxpayers fund basic research of a drug, they deserve more of the control--and rewards--when that drug succeeds.
Trump and Musk are on an unconstitutional rampage, aiming for virtually every corner of the federal government. These two right-wing billionaires are targeting nurses, scientists, teachers, daycare providers, judges, veterans, air traffic controllers, and nuclear safety inspectors. No one is safe. The food stamps program, Social Security, Medicare, and Medicaid are next. It’s an unprecedented disaster and a five-alarm fire, but there will be a reckoning. The people did not vote for this. The American people do not want this dystopian hellscape that hides behind claims of “efficiency.” Still, in reality, it is all a giveaway to corporate interests and the libertarian dreams of far-right oligarchs like Musk. Common Dreams is playing a vital role by reporting day and night on this orgy of corruption and greed, as well as what everyday people can do to organize and fight back. As a people-powered nonprofit news outlet, we cover issues the corporate media never will, but we can only continue with our readers’ support. |
A quiet monthslong legal fight between the U.S. National Institutes of Health and drugmaker Moderna over COVID-19 vaccine patents recently burst into public view. The outcome of the battle has important implications, not only for efforts to contain the pandemic but more broadly for drugs and vaccines that could be critical for future public health crises.
I teach drug regulation and patent law at Saint Louis University's Center for Health Law Studies.
Moderna recently offered to share ownership of its main patent with the government to resolve the dispute. Whether or not this is enough to satisfy the government's claims, I believe the dispute points to serious problems in the ways U.S. companies bring drugs and vaccines to market.
Vaccines have played a crucial role in the response to the pandemic.
In December 2020, Moderna became the second pharmaceutical company after Pfizer to obtain authorization from the Food and Drug Administration to market a COVID-19 vaccine in the United States. People have since grown so used to talking about the "Moderna vaccine" that a crucial element in the history of how it was developed risks being overshadowed: Moderna was not the sole developer of the vaccine.
Unlike many of the other pharmaceutical companies involved in the COVID-19 vaccine race, Moderna is a newcomer to drug and vaccine commercialization. Founded in Massachusetts in 2010, the company had never brought a product to market until the FDA authorized its COVID-19 vaccine last year.
Throughout the 2010s, Moderna focused on the development of mRNA technology, attracting over US$2 billion in funding from pharmaceutical companies and other investors. It went public in 2018.
Even before the pandemic, research on both coronaviruses and vaccine candidates against emerging pathogens was a priority for agencies operating in the public health space. In 2015, the National Institute of Allergy and Infectious Diseases, an institute within the NIH, signed a cooperative R&D agreement with Moderna on basic research, including the development of new vaccines. The agreement resulted in an undisclosed amount of funding and assistance with research.
In addition, after the COVID-19 outbreak began Moderna also received almost $1 billion in funding from the Biomedical Advanced Research and Development Authority, which operates within the Department of Health and Human Services. This funding was specifically targeted to the development of a COVID-19 vaccine candidate.
Researchers have calculated that, collectively, the U.S. government has provided $2.5 billion toward the development and commercialization of Moderna's COVID-19 vaccine.
In addition to providing financial support, the federal government was instrumental in the development of Moderna's vaccine for other reasons. Namely, federal scientists worked alongside Moderna scientists on different components of the vaccine.
These contributions included working on dosing mechanisms, and the NIH said federal scientists created the stabilized spike proteins that are a key component of the vaccine made by Moderna.
The importance of the role played by federal scientists in their work with Moderna would soon become apparent. A 2019 agreement with a third party explicitly acknowledged this, alluding to mRNA vaccine candidates "developed and jointly owned by NIAID and Moderna." And by late 2020, the U.S. government was calling it the "NIH-Moderna COVID-19 vaccine."
While the U.S. government has spent money on COVID-19 vaccines made by other companies, its close involvement in the R&D stages of Moderna's sets it apart.
As development of the vaccine progressed, Moderna applied for several patents, each one covering different components of the vaccine. U.S. law allows inventors to apply for patents on products or methods that are new, not obvious and useful. While some early modern vaccines--like the polio vaccine developed by Jonas Salk's team--were not covered by patents, from the late 20th century onward it became very common for one or multiple patents to cover a newly developed vaccine.
In applying for some patents related to its vaccine, Moderna named National Institute of Allergy and Infectious Diseases scientists as co-inventors alongside Moderna scientists. This was the case, for example, in a patent application dated May 2020 for a relatively minor component of the vaccine.
However, in July 2021, Moderna made it clear that it would not name government scientists as co-inventors in a patent application covering a much more significant component of the vaccine: the mRNA sequence used to produce the vaccine, known as mRNA-1273.
Moderna's position was that Moderna scientists alone had selected the sequence. The company informed the Patent and Trademark Office of its position in a 2020 statement.
In November 2021, government officials publicly challenged the company's decision after months of failed negotiations with the company. Moderna then took to social media to defend its position, tweeting:
"Just because someone is an inventor on one patent application relating to our COVID-19 vaccine does not mean they are an inventor on every patent application relating to the vaccine."
\u201cOur official statement on intellectual property. Thread.\u201d— Moderna (@Moderna) 1636663102
By contrast, the National Institutes of Health argued that three NIAID scientists--Kizzmekia Corbett, Barney Graham and John Mascola--had meaningfully contributed to the invention, though they've declined to publicly specify how. If true, patent law says they should be named co-inventors.
But this dispute is not merely about scientific principles or technical aspects of the law. While patents are also regarded as proxies for measuring scientific reputation, their most immediate and powerful effect is to give patent holders a significant amount of control over the covered technology--in this case, the main component of the vaccine made by Moderna.
From a practical perspective, excluding federal scientists from the application means that Moderna alone gets to decide how to use the vaccine, whether to license it and to whom. If, by contrast, the government co-owns the vaccine, federal patent law allows each of the joint owners to engage in a variety of actions--from making and selling the vaccine to licensing it--without the consent of the other owners.
This is especially relevant in cases of product scarcity or potential pricing issues in connection with the commercialization of the vaccine. For instance, the U.S. would have the ability to allow more manufacturers to produce vaccines using the mRNA-1273 technology. In addition, it could direct vaccine doses wherever it likes, including to lower-income countries that have received few vaccines so far.
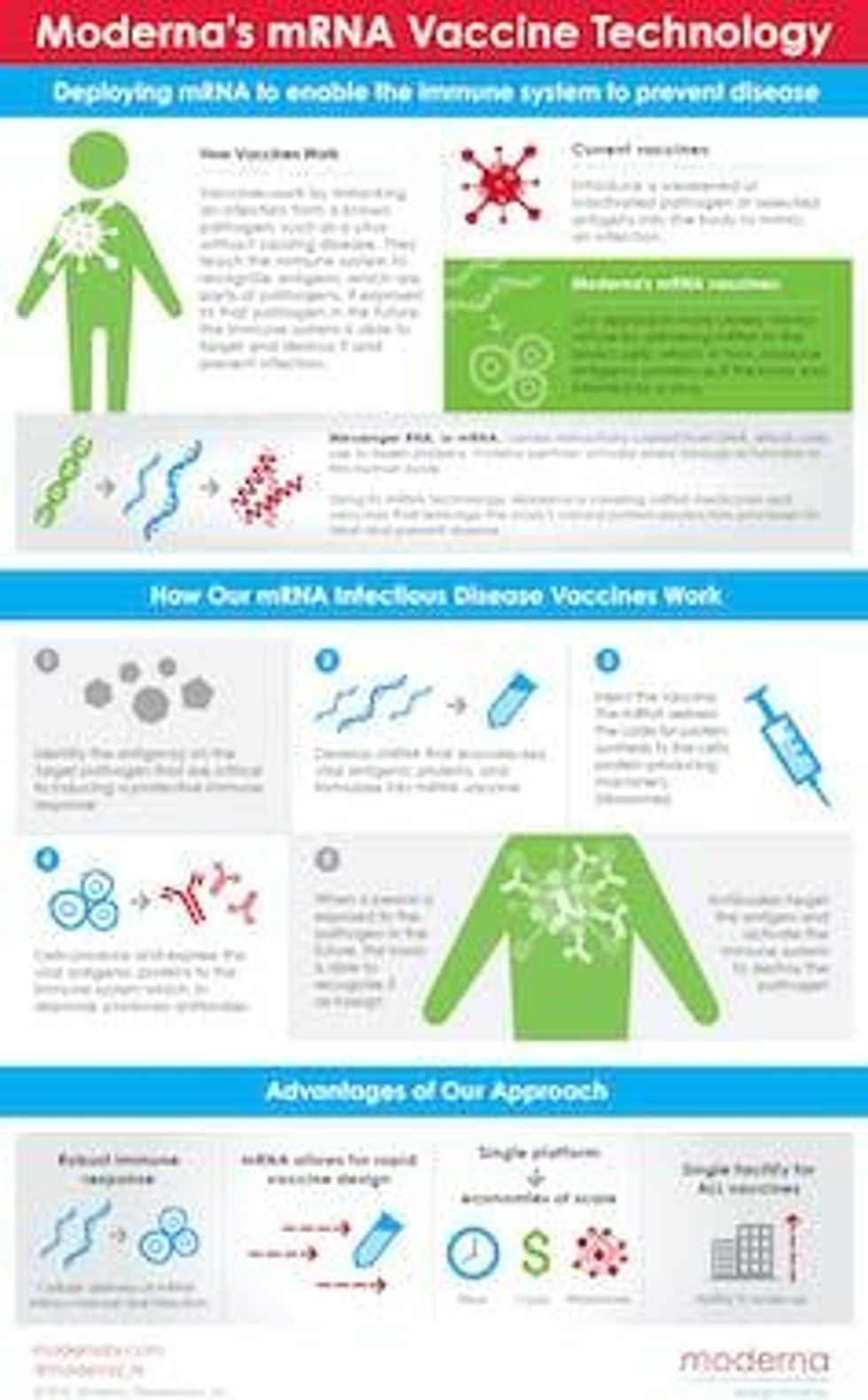 Moderna explains its mRNA technology. (Business Wire)
Moderna explains its mRNA technology. (Business Wire)The ongoing battle between the government and an emerging star in the pharmaceutical industry is yet another episode in a complicated relationship between actors with complementary yet distinct roles in the production of drugs and vaccines.
On the one hand, the federal government has long played a critical role in both performing and funding basic research. On the other, it does not have the resources and capacity to bring most types of new drugs and vaccines to market on its own.
The pharmaceutical industry thus plays an important and necessary role in drug innovation, which I believe should be rewarded--although not boundlessly.
If the NIH is correct about co-ownership of the vaccine, then Moderna is unduly using a legal tool to achieve a position of market control--a reward it does not deserve. This position of sole control becomes even more problematic in light of the significant amounts of public money that funded the development of this vaccine. This offset some of Moderna's financial risk, even as the company projects to make $15 billion to $18 billion in revenue from vaccine sales in 2021 alone, with much more expected in 2022.
However, even if the NIH prevails in the patent dispute, it is important to understand the limitations of such a "win." The U.S. would be in a position to license the vaccine, for example, and could do so by requiring that licensees agree to equitable distribution of vaccine doses.
But co-ownership would not enable the government to fix any of the other problems that currently affect the manufacturing and distribution of COVID-19 vaccines, such as scaling up production or building infrastructure to deliver vaccine doses.
In my view, the dispute is a reminder of the many problems embedded in how vaccines are made and delivered in the U.S. And it shows that when taxpayers fund basic research of a drug, they deserve more of the control--and rewards--when that drug succeeds.
A quiet monthslong legal fight between the U.S. National Institutes of Health and drugmaker Moderna over COVID-19 vaccine patents recently burst into public view. The outcome of the battle has important implications, not only for efforts to contain the pandemic but more broadly for drugs and vaccines that could be critical for future public health crises.
I teach drug regulation and patent law at Saint Louis University's Center for Health Law Studies.
Moderna recently offered to share ownership of its main patent with the government to resolve the dispute. Whether or not this is enough to satisfy the government's claims, I believe the dispute points to serious problems in the ways U.S. companies bring drugs and vaccines to market.
Vaccines have played a crucial role in the response to the pandemic.
In December 2020, Moderna became the second pharmaceutical company after Pfizer to obtain authorization from the Food and Drug Administration to market a COVID-19 vaccine in the United States. People have since grown so used to talking about the "Moderna vaccine" that a crucial element in the history of how it was developed risks being overshadowed: Moderna was not the sole developer of the vaccine.
Unlike many of the other pharmaceutical companies involved in the COVID-19 vaccine race, Moderna is a newcomer to drug and vaccine commercialization. Founded in Massachusetts in 2010, the company had never brought a product to market until the FDA authorized its COVID-19 vaccine last year.
Throughout the 2010s, Moderna focused on the development of mRNA technology, attracting over US$2 billion in funding from pharmaceutical companies and other investors. It went public in 2018.
Even before the pandemic, research on both coronaviruses and vaccine candidates against emerging pathogens was a priority for agencies operating in the public health space. In 2015, the National Institute of Allergy and Infectious Diseases, an institute within the NIH, signed a cooperative R&D agreement with Moderna on basic research, including the development of new vaccines. The agreement resulted in an undisclosed amount of funding and assistance with research.
In addition, after the COVID-19 outbreak began Moderna also received almost $1 billion in funding from the Biomedical Advanced Research and Development Authority, which operates within the Department of Health and Human Services. This funding was specifically targeted to the development of a COVID-19 vaccine candidate.
Researchers have calculated that, collectively, the U.S. government has provided $2.5 billion toward the development and commercialization of Moderna's COVID-19 vaccine.
In addition to providing financial support, the federal government was instrumental in the development of Moderna's vaccine for other reasons. Namely, federal scientists worked alongside Moderna scientists on different components of the vaccine.
These contributions included working on dosing mechanisms, and the NIH said federal scientists created the stabilized spike proteins that are a key component of the vaccine made by Moderna.
The importance of the role played by federal scientists in their work with Moderna would soon become apparent. A 2019 agreement with a third party explicitly acknowledged this, alluding to mRNA vaccine candidates "developed and jointly owned by NIAID and Moderna." And by late 2020, the U.S. government was calling it the "NIH-Moderna COVID-19 vaccine."
While the U.S. government has spent money on COVID-19 vaccines made by other companies, its close involvement in the R&D stages of Moderna's sets it apart.
As development of the vaccine progressed, Moderna applied for several patents, each one covering different components of the vaccine. U.S. law allows inventors to apply for patents on products or methods that are new, not obvious and useful. While some early modern vaccines--like the polio vaccine developed by Jonas Salk's team--were not covered by patents, from the late 20th century onward it became very common for one or multiple patents to cover a newly developed vaccine.
In applying for some patents related to its vaccine, Moderna named National Institute of Allergy and Infectious Diseases scientists as co-inventors alongside Moderna scientists. This was the case, for example, in a patent application dated May 2020 for a relatively minor component of the vaccine.
However, in July 2021, Moderna made it clear that it would not name government scientists as co-inventors in a patent application covering a much more significant component of the vaccine: the mRNA sequence used to produce the vaccine, known as mRNA-1273.
Moderna's position was that Moderna scientists alone had selected the sequence. The company informed the Patent and Trademark Office of its position in a 2020 statement.
In November 2021, government officials publicly challenged the company's decision after months of failed negotiations with the company. Moderna then took to social media to defend its position, tweeting:
"Just because someone is an inventor on one patent application relating to our COVID-19 vaccine does not mean they are an inventor on every patent application relating to the vaccine."
\u201cOur official statement on intellectual property. Thread.\u201d— Moderna (@Moderna) 1636663102
By contrast, the National Institutes of Health argued that three NIAID scientists--Kizzmekia Corbett, Barney Graham and John Mascola--had meaningfully contributed to the invention, though they've declined to publicly specify how. If true, patent law says they should be named co-inventors.
But this dispute is not merely about scientific principles or technical aspects of the law. While patents are also regarded as proxies for measuring scientific reputation, their most immediate and powerful effect is to give patent holders a significant amount of control over the covered technology--in this case, the main component of the vaccine made by Moderna.
From a practical perspective, excluding federal scientists from the application means that Moderna alone gets to decide how to use the vaccine, whether to license it and to whom. If, by contrast, the government co-owns the vaccine, federal patent law allows each of the joint owners to engage in a variety of actions--from making and selling the vaccine to licensing it--without the consent of the other owners.
This is especially relevant in cases of product scarcity or potential pricing issues in connection with the commercialization of the vaccine. For instance, the U.S. would have the ability to allow more manufacturers to produce vaccines using the mRNA-1273 technology. In addition, it could direct vaccine doses wherever it likes, including to lower-income countries that have received few vaccines so far.
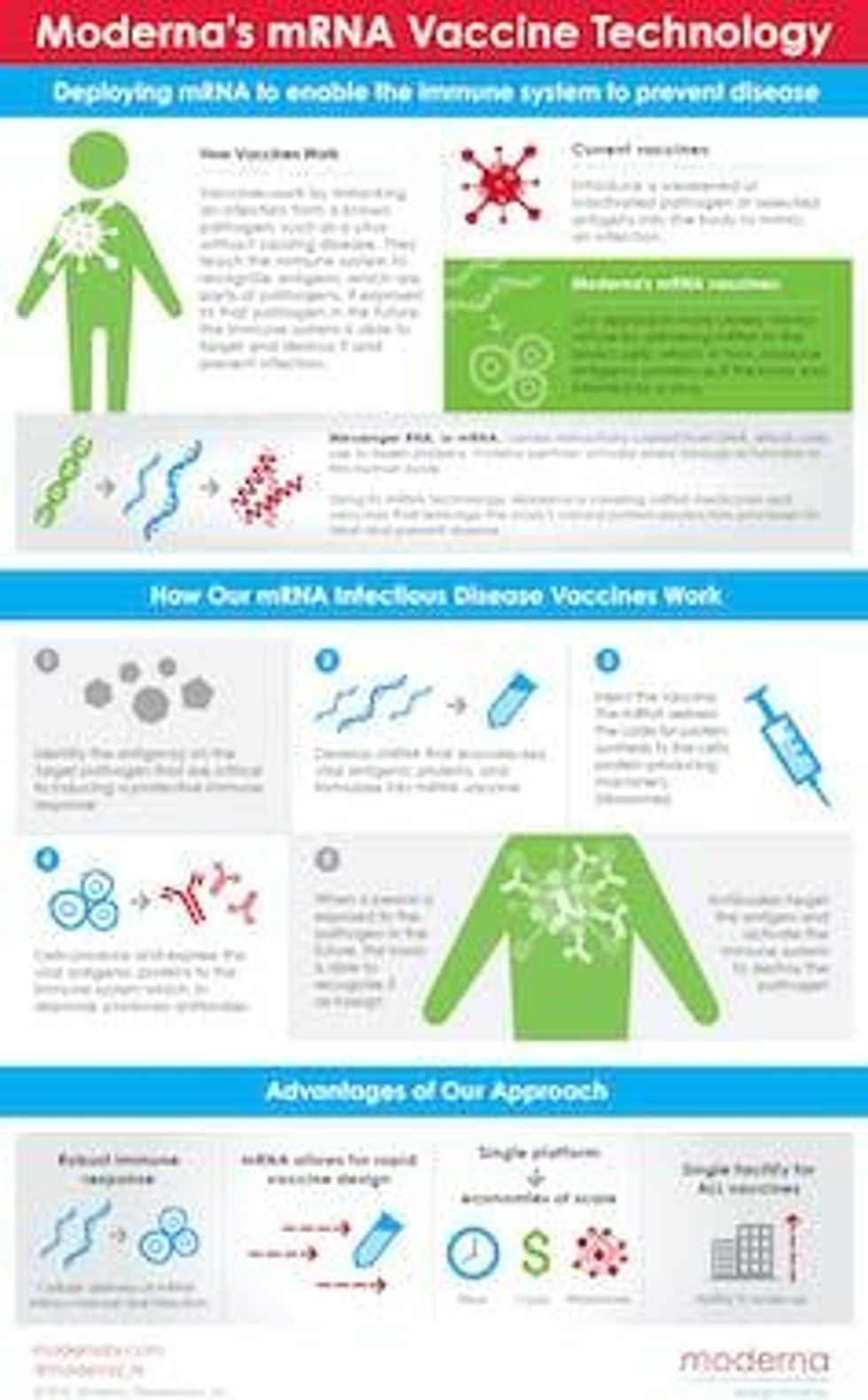 Moderna explains its mRNA technology. (Business Wire)
Moderna explains its mRNA technology. (Business Wire)The ongoing battle between the government and an emerging star in the pharmaceutical industry is yet another episode in a complicated relationship between actors with complementary yet distinct roles in the production of drugs and vaccines.
On the one hand, the federal government has long played a critical role in both performing and funding basic research. On the other, it does not have the resources and capacity to bring most types of new drugs and vaccines to market on its own.
The pharmaceutical industry thus plays an important and necessary role in drug innovation, which I believe should be rewarded--although not boundlessly.
If the NIH is correct about co-ownership of the vaccine, then Moderna is unduly using a legal tool to achieve a position of market control--a reward it does not deserve. This position of sole control becomes even more problematic in light of the significant amounts of public money that funded the development of this vaccine. This offset some of Moderna's financial risk, even as the company projects to make $15 billion to $18 billion in revenue from vaccine sales in 2021 alone, with much more expected in 2022.
However, even if the NIH prevails in the patent dispute, it is important to understand the limitations of such a "win." The U.S. would be in a position to license the vaccine, for example, and could do so by requiring that licensees agree to equitable distribution of vaccine doses.
But co-ownership would not enable the government to fix any of the other problems that currently affect the manufacturing and distribution of COVID-19 vaccines, such as scaling up production or building infrastructure to deliver vaccine doses.
In my view, the dispute is a reminder of the many problems embedded in how vaccines are made and delivered in the U.S. And it shows that when taxpayers fund basic research of a drug, they deserve more of the control--and rewards--when that drug succeeds.